Rheumatology Billing – Precision for Chronic Care
Our billing solutions help rheumatology practices improve cash flow and minimize revenue leakage.
Specialized in Rheumatology Billing – Covering infusions, joint injections, and consultations.
Optimized Revenue Streams – Ensure timely reimbursements with accurate coding.
Seamless RCM & Claim Tracking – Reduce administrative burden.
Data Protection & HIPAA Compliance – Ensuring secure patient information handling.
LET'S GET STARTED
We Are Looking Forward to Hear from You..!!


WHY EVOCARE BILLINGS...??










Comprehensive Eligibility & Benefits Verification
We streamline prior authorizations and benefits verification to prevent claim denials and ensure smooth reimbursements.
Strict HIPAA Compliance & Data Security
Proactive Denial Prevention & Management
Seamless EHR Compatibility
Performance Analytics & Revenue Optimization
Expert Billing Support You Can Trust
We prioritize patient confidentiality and financial security with 100% HIPAA-compliant processes.
Minimize revenue loss with our robust claim scrubbing, resubmission strategies, and denial resolution expertise.
Gain valuable insights with our customized reports, allowing you to track revenue trends and improve financial strategies.
Our billing solutions integrate with various EHR systems, ensuring efficiency and compliance for your practice.
With a team of certified professionals and years of industry experience, we help maximize your practice’s profitability.

Our Success In Numbers
We are dealing with the clients since a long time
$125M+
Value of Claims Processed
Since 2019
99%
Total Revenue Collected
24
Accounts Receivable Days
48 Hours
Turn Around Time
1,000,000+
Number Of Claims Processed
99%
Customer Retention
98%
First Pass Clean Claim Rate
15-20%
Revenue Improvement
26 Days
Turn Around Time For Payment
35%
Reduction In Accounts Receivable
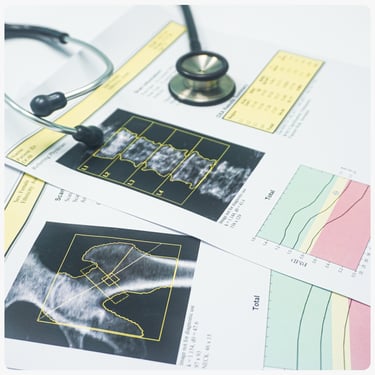
Resilient Rheumatology Medical Billing Strengthening Accuracy and Regulatory Adherence
Resilient Rheumatology Medical Billing Strengthening Accuracy and Regulatory Adherence
Rheumatology medical billing requires precision in coding and compliance due to the complexity of chronic disease management. Incorrect documentation and coding errors can lead to higher claim denials, affecting revenue streams. With over 20% of rheumatology claims facing rejections annually (AAPC, 2023), accurate billing and adherence to payer guidelines are critical. Advanced coding strategies ensure correct reimbursement for biologic therapies, infusions, and disease-modifying treatments. Automated verification of patient eligibility and benefits further streamlines the billing process. Outsourcing rheumatology billing to certified experts reduces administrative burdens, allowing physicians to focus on patient care.
Reducing Denials and Increasing Reimbursements for Rheumatology Practices
Claim denials in rheumatology often stem from incorrect coding of infusion services, lack of medical necessity documentation, or payer policy updates. Addressing these challenges requires a strategic billing approach with regular training on coding updates. Expert billing teams ensure accurate use of CPT codes for infusion therapy and musculoskeletal procedures, reducing billing errors. An efficient revenue cycle management (RCM) system identifies underpayments and initiates timely appeals. Implementing a robust compliance framework minimizes legal risks and enhances financial performance.

Implementation of accurate coding for disease-modifying anti-rheumatic drugs (DMARDs) and biologic therapies.
Ensuring compliance with payer policies to prevent claim rejections and audits.
Proactive claim scrubbing to identify and correct potential coding errors.
Prior authorization management for biologic infusions and injectable medications.
Regular follow-ups on pending claims to minimize revenue loss.
Streamlined documentation and EHR integration to enhance billing efficiency.
Regular audits to ensure correct documentation and coding compliance.
Automated eligibility checks to prevent claim rejections due to insurance issues.
Proactive tracking of underpaid claims and timely resubmission.
Utilization of AI-driven tools for accurate charge capture and revenue forecasting.
Compliance monitoring to adhere to CMS and commercial payer guidelines.
Patient-friendly billing strategies to enhance collections and reduce bad debt.
What Our Clients Say?


Evo Care Medical Billing has been a game-changer for our practice. Their expertise in Chronic Care Management (CCM) helped us significantly increase patient enrollments, resulting in an incredible 233% revenue growth within six months. Their team streamlined our workflow, improved patient engagement, and ensured compliance, making a lasting impact on our success. We highly recommend their services to any healthcare provider looking to optimize billing and patient care.
Diane Baucom- Chronic Care Manager - AIMS Florida














Earn more and get paid faster with Evocare Medical Billing's 24/7 services.
Evocare is a medical billing provider that integrates with your existing EHR system for streamlined processing.
We are honored to offer top-tier service with a 99% retention rate that sets us apart.